- Home
- Intrauterine Insemination(IUI)
In vitro Fertilization (IVF/ET)
Commonly known as “test-tube babies”, IVF/ET involves harvesting (mature) eggs from the woman’s ovaries, fertilizing these eggs with the man’s sperms outside the body, culturing these fertilized eggs in the laboratory until 3 to 5 days before returning them (known as “cleavage stage embryos” or “blastocysts” respectively) to the woman’s womb. The world’s first IVF baby, Louise Brown, was born in 1978. The treatment was originally intended to help women with blocked or missing (fallopian) tubes to conceive but has since been used to treat all causes of infertility (vide infra).
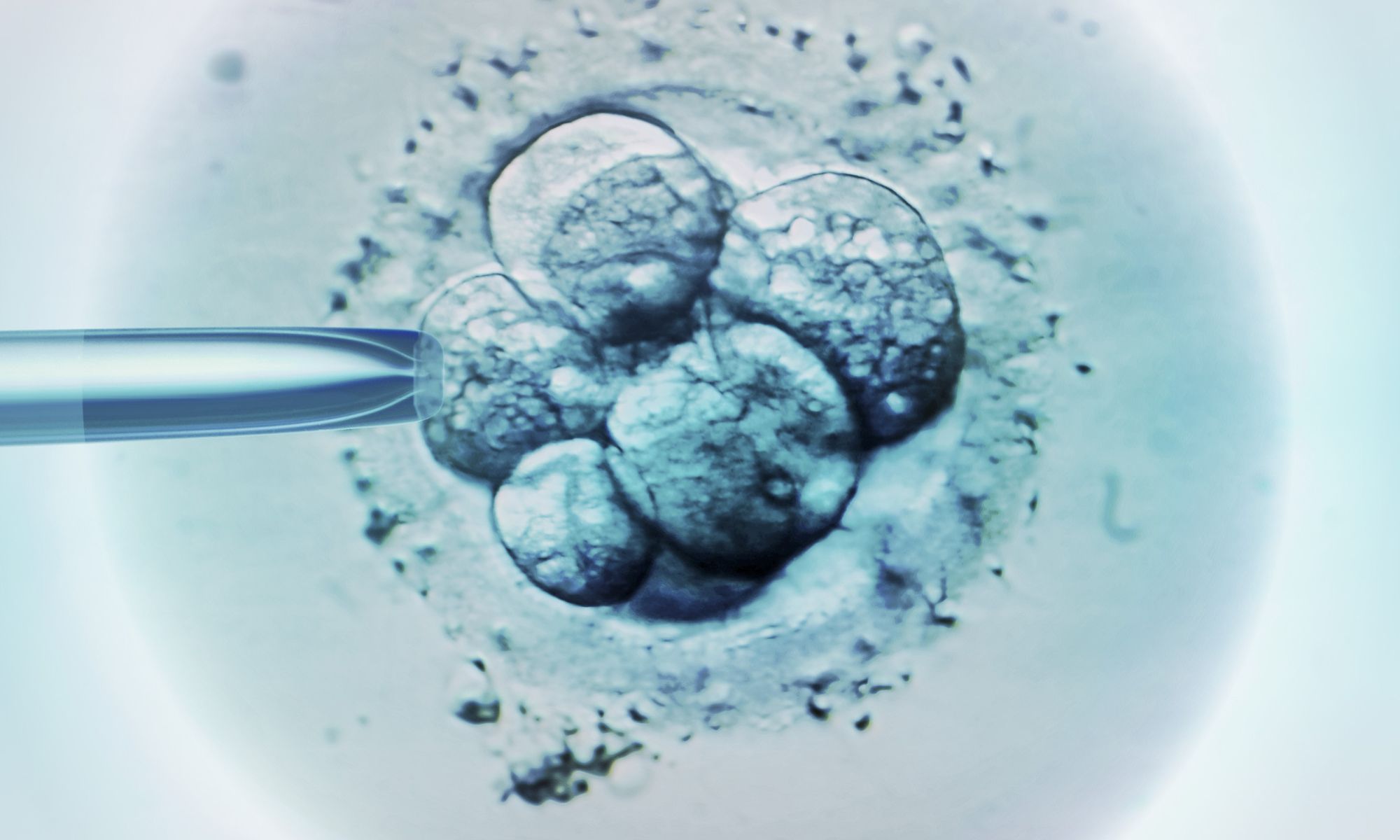
According to estimates, over 5 million babies have been born using IVF worldwide. Over the past three decades, children conceived by in vitro fertilization have not been found to have increased risk of birth defects. More recent and larger studies appear to indicate that there is a higher risk of genitourinary, cardiovascular, musculoskeletal and chromosomal abnormalities in IVF and IVF(ICSI) offspring but researchers have yet to separate out the “chicken or egg” issue, i.e., whether the procedure of in vitro fertilization or infertility itself is the true culprit. Other studies have also suggested that the higher risk of birth defects is associated with intra-cytoplasmic sperm injection (ICSI) (vide infra) and not IVF.
Indications for in vitro fertilization include tubo-peritoneal disease, unexplained or idiopathic infertility, particularly after repeated IUI failures, severe male factor infertility – triple sperm defects i.e. oligo-astheno-teratozoospermia (OAT), severe pelvic endometriosis and sometimes in advanced female age and diminished ovarian reserve.